(Spoiler: We Needed a Code Cart for Supplies, Not Patients)
Children are supposed to bring bright drawings and contagious laughter.
Mine brought silence.
The moment you bring your kid to work — and that work happens to be the ICU — the air shifts.
Monitors beep.
Ventilators hiss.
One of the nurses made the sign of the cross, very subtly, behind a rolling supply cart.
It wasn’t because my child was misbehaving.
It was because no one, in the history of this unit, had willingly exposed a small, innocent human being to the full existential horror that is a critical care ward before lunchtime.
“She’ll just stay in the corner and color,” I promised.
At that precise moment, a code blue echoed through the hall.
Coloring was canceled.
Existentialism was fully activated.
My daughter, unfazed, sat quietly in a folding chair as a parade of very serious people moved in and out of trauma.
She watched someone reintubate a patient like she was watching a slightly boring magic show.
She took a juice box break while I held pressure on an arterial line.
At one point she looked up from her crayons and said:
“Mommy, that man’s numbers are going down. That’s bad, right?”
Absolutely correct, sweetheart.
Welcome to critical care.
Here’s your complimentary PTSD starter kit.
When you bring your kid to work at a place like this, you don’t leave with drawings.
You leave with a weird, solemn little warrior who thinks near-death experiences are part of the schedule.
When we finally left, she gave the ICU a polite wave goodbye —
like she was leaving a mildly disappointing birthday party.
No balloons. No cake. Just blood, adrenaline, and the slow, grim satisfaction of survival.
She still thinks it was “kind of cool.”
I have never fully recovered.
Table of Contents
If you think bring your kid to work sounds chaotic, wait until you see what surgeons say about their own disasters — 10 memorable quotes about surgery explain everything.
My Boss Called … On My Day Off
When my boss called, I explained — very reasonably — that it was my day off, and that my child was at home because there was no one to watch her.
She paused.
Then she said the sacred ICU phrase:
“However you decide.”
Which, for those fluent in passive-aggressive healthcare dialects, translates directly to:
“I don’t like your attitude, and I expect you to show up anyway.”
So naturally, when my deeply malfunctioning moral compass refused to let my coworkers bleed out alone on the ICU battlefield —
with eight OR rooms blazing and alarms screaming —
I made the only logical choice left:
grabbed my toddler, threw her into a jacket, and marched straight into the chaos.
Because in critical care, the options are always:
- Betray your team.
- Sacrifice your sanity.
Choose wisely.
The Entry of a Tiny Civilian
She entered the ICU like she had been summoned.
Tiny teal scrubs perfectly pressed, a plastic stethoscope bouncing on her chest, Velcro sneakers squeaking with every fearless step.
Eyes serious. Chin high.
The smallest, most confident healthcare provider the unit had ever seen.
Every head turned.
Every monitor seemed to beep softer, like even the machines were trying to make a good impression.
There were protocols for everything —
for crashing airways, exploding chests, unsalvageable rhythms.
But nowhere in the sterile, color-coded survival manuals was there a section titled:
“What to do when you bring your kid to work and she actually reports for duty.”
And God help them all —
they were happy to see her.
Because when you’re buried under alarms and ventilators and another two cases waiting for ICU beds,
even a three-foot-tall civilian looks like hope wearing glittery sneakers.
They smiled.
They laughed.
They made space for her like she was a good omen.
Little did they know, they had just voluntarily admitted a walking disaster into critical care.
After a day like this, bring your kid to work probably deserves its own diagnosis — something straight out of these funny medical condition names we wish were real.
Collateral Damage
It didn’t take long for the smiles to fade.
Five minutes after her grand entrance, I was trapped in the OR — masked, gowned, tethered to an anesthesia machine, keeping someone marginally attached to life.
Exactly the kind of moment where chasing down your rogue toddler is frowned upon.
I left her under the unofficial custody of the ICU nurses —
a team that could crack open a chest in under two minutes but apparently wasn’t prepared for what was about to unfold.
The first warning came fast and loud.
A nurse burst through the OR door, eyes wide, breathless, full panic in her voice:
“Drs. Sat Drop! She extubated Bed 3! He’s breathing, but he’s furious! We’re bagging him manually!”
The room froze.
For a second, even the surgeons paused — scalpels midair, disbelief written across their faces.
I couldn’t move.
I couldn’t leave.
I could only nod grimly and signal for them to keep going.
Another ten minutes.
Another frantic call.
“Drs. Sat Drop, your kid pulled out Mr. Teddy Bear’s chest drain. He’s bleeding. We’re containing it. Sort of.”
Muffled suctioning noises in the background.
Someone cursing very quietly.
Five minutes later:
“She climbed onto Bed 6. He’s sedated, but it’s… it’s not ideal, Doctor.”
At that point, we stopped pretending this was normal.
We simply adapted — as all critical care people eventually do when life hands them absurdity wrapped in sparkling sneakers.
By the time we rolled the patient to recovery, the ICU looked like the losing end of a minor war —
battered staff, half-repaired patients, and my daughter calmly coloring at the nurses’ station,
blissfully unaware she had personally added three critical incidents to the shift report.
Bring your kid to work was supposed to be about showing them what you do.
Mine decided to wreak strategic, full-scale havoc instead.
Negotiations Begin
At first, they tried stickers.
Someone found an ancient roll in the supply closet — half-faded, curling at the edges — and offered them up like sacred relics.
She accepted them solemnly, plastered two on her stethoscope, and immediately wandered off toward Bed 5 with the focused energy of a surgeon preparing for a high-risk procedure.
Next came the pens.
Brightly colored, retractable, irresistible.
A nurse surrendered a whole handful, hoping to buy five minutes of peace.
She took the pens, nodded gravely, and used them to chart “notes” in a patient’s progress report —
directly on the actual chart.
In crayon.
After that, they tried bribes.
“Sweetheart, if you sit here and color, you can have a snack.”
“Look, here’s a real stethoscope — it’s heavy, it’s shiny!”
“Want to press the ventilator buttons? No? Okay, good, let’s not.”
At one point, an entire care plan for a crashing patient was negotiated around her movements —
two nurses exchanging a silent agreement that one would bag the sedated patient while the other intercepted my daughter mid-sprint before she reached the code cart.
It became a full-blown tactical operation:
“You distract her, I’ll tie down the chest tube.”
“I’ll read her a story if you grab the IV pole.”
“Somebody get her a juice box, she’s entering Zone Red.”
By Hour Two, hardened ICU veterans — people who had manually massaged dying hearts back to life — were visibly sweating under the pressure of keeping one determined toddler from inadvertently committing felonies.
It turns out that when you bring your kid to work, you don’t just bring crayons and juice boxes.
You bring an unstoppable biological weapon into critical care.
And somehow, impossibly, the ICU stayed upright.
Barely.
At least until the crayons ran out.
Honestly, bring your kid to work feels almost as dangerous as taking a 15-minute lunch break and coming back with a lawsuit — short break, long consequences.
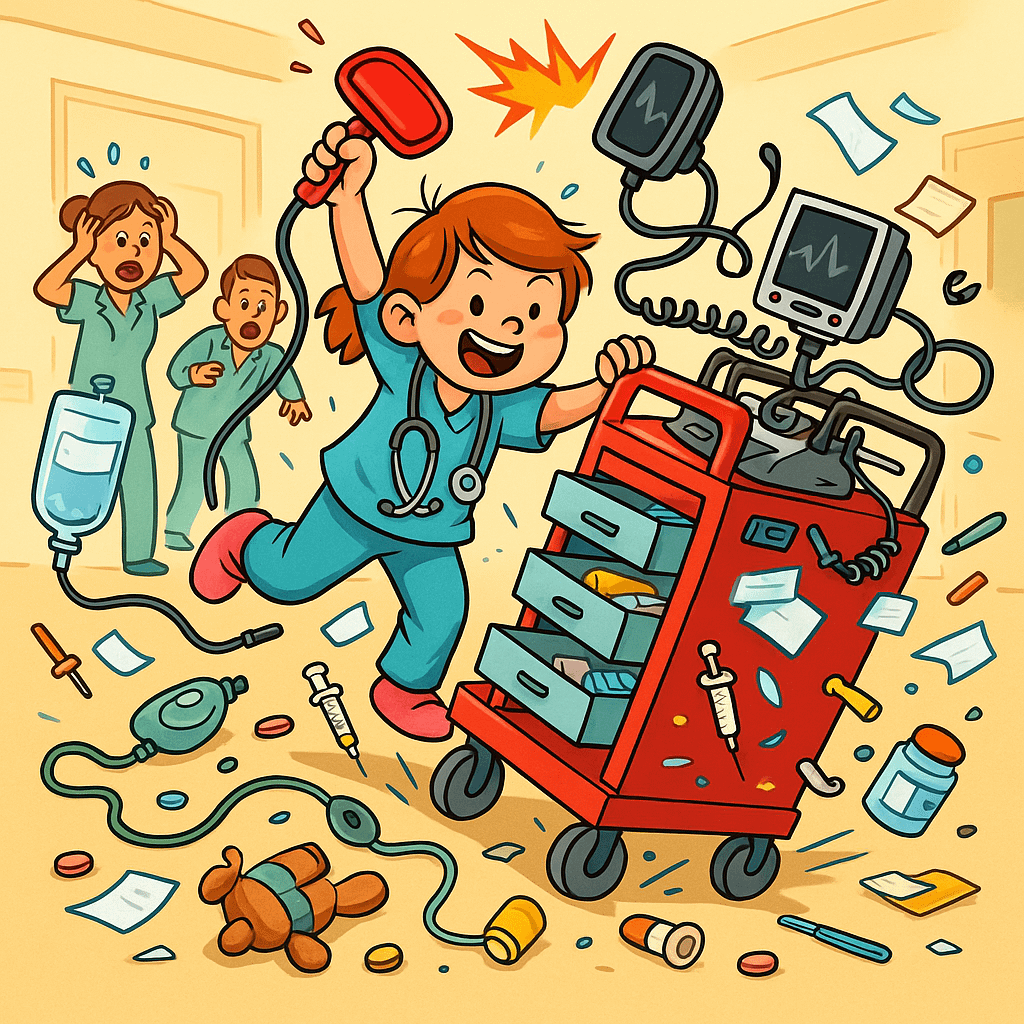
The Crash Cart Needed A Crash Cart
Despite my desperate pre-shift crash course in ICU survival —
“Don’t touch anything sharp. Don’t pull anything red. Don’t drink anything blue.” —
it turns out that when you bring your kid to work, they don’t see emergency equipment.
They see a playground.
She took one look at the emergency crash cart and decided it needed a full renovation.
Within twenty minutes, she had reordered half the drawers.
Syringes stacked by color instead of size.
Airway equipment sorted by how “shiny” it looked, not by urgency.
The defibrillator pads were peeled, examined, and repurposed into wall stickers.
Then she found a handful of discarded pediatric ECG electrodes —
and in an inspired moment of interior design, decorated the side of the crash cart with tiny sparkling smiley faces.
Emergency drugs were alphabetized…
sort of.
Only now, adrenaline lived next to apple juice (in her mind), and atropine was apparently filed under “A” for “Awesome.”
By the time anyone noticed,
the crash cart looked less like a life-saving station and more like an unsupervised art project.
A project that, if rolled into an actual code, would have either saved a life in record time —
or ended one with spectacular, crayon-enhanced efficiency.
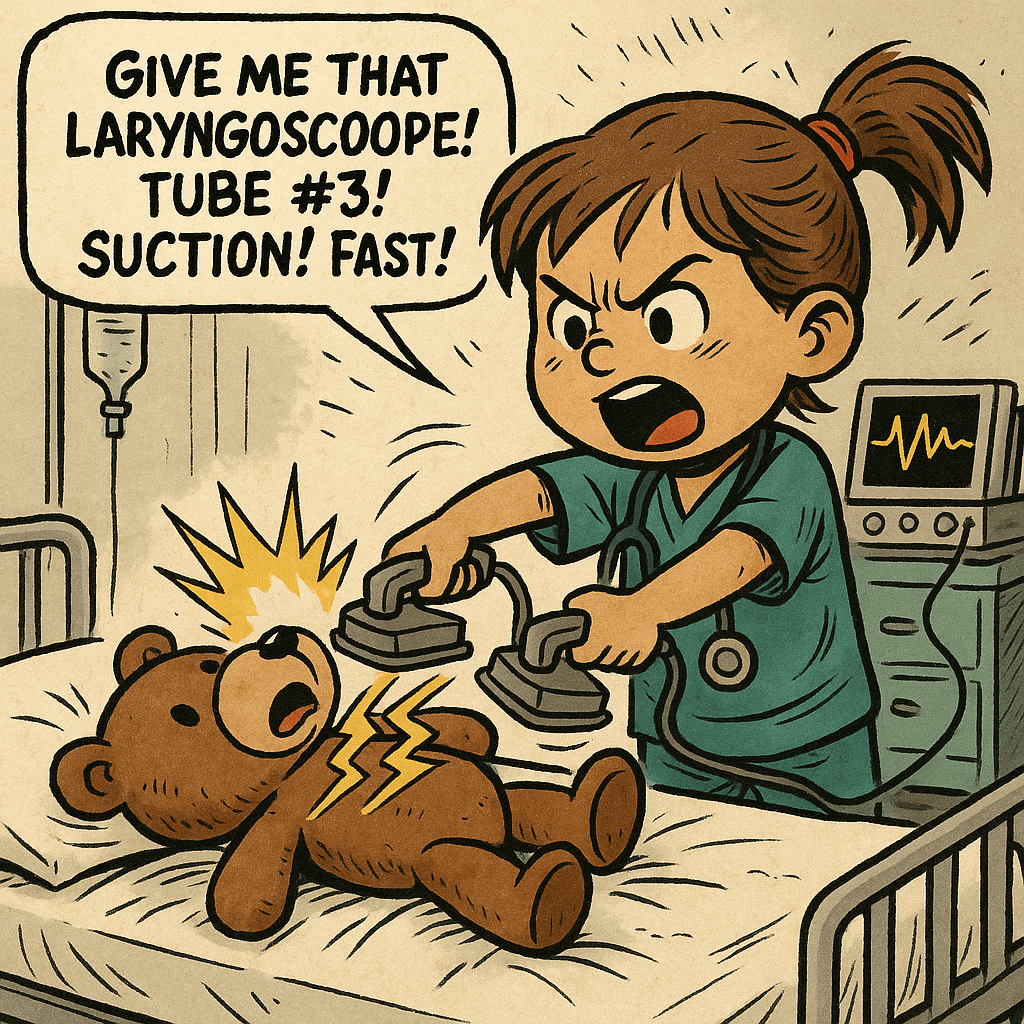
Clear. Again. And Again.
At some point — no one is exactly sure when —
she found an old teddy bear tucked behind the nurses’ station.
And because she had been observing very closely,
and because toddlers don’t believe in equipment checks or medical licensing,
she decided the bear needed defibrillation.
Immediately.
Repeatedly.
She dragged the bear onto an empty stretcher, positioned it with expert care,
and began issuing orders at full ICU code volume:
“Charging! Clear!”
SLAM.
“Charging again! Clear!”
SLAM.
Then it escalated.
“Give me that laryngoscope!” she bellowed, hand snapping open with authority.
“Tube! Size three! Hurry! He’s desaturating!”
“Suction! Where’s suction?! MOVE!”
“WHERE’S RESPIRATORY?!”
One of the nurses instinctively started reaching for the intubation tray —
caught halfway between obeying and realizing the “patient” was a teddy bear and the “team leader” was four years old.
It was at that exact moment —
amidst tiny feet stomping for suction and a bear being manually ventilated with imaginary air —
that my boss walked into the ICU.
She froze.
The scene unfolded before her:
a child in miniature scrubs screaming critical orders, a fully staffed unit half-heartedly following them,
and a teddy bear receiving the best resuscitation support in the building.
I had brought my kid to work —
and in the purest, most catastrophic sense imaginable,
she had taken over.
For a long moment, my boss just stood there.
No words.
No movement.
Just the slow, dawning horror of realizing that “bring your kid to work” had evolved into “initiate pediatric hostile takeover.”
Finally, she whispered — mostly to herself —
“I need a vacation.”
Nobody disagreed.
If you think bring your kid to work causes chaos, wait until you hear these pickup lines for nurses that should absolutely be illegal.
We Lost a Cart Today
By the end of the shift, the crash cart looked worse than some of the patients.
Defibrillator pads peeled half off, syringes scattered like fallen soldiers, IV start kits jammed into the wrong drawers.
Someone had written “good luck” inside the airway box in crayon.
The cart didn’t roll straight anymore.
It leaned slightly to the left, like it, too, had seen too much and decided full functionality was optional.
It turns out that when you bring your kid to work,
you don’t just risk your sanity —
you also risk the structural integrity of critical care equipment.
Technically, all the necessary supplies were still present.
Technically, it could still be used in an emergency.
Realistically, you’d have a better shot at saving someone by swinging the entire thing at them like a battering ram.
We called it.
Time of death: five minutes after my daughter performed her third teddy bear resuscitation.
Cause: exposure to unfiltered toddler enthusiasm and unregulated ICU creativity.
Nobody even tried to fix it that day.
We just pushed it into a corner and looked away.
Not It. Forever
In the end, everyone survived.
Most of the patients.
Most of the staff.
The equipment… needed counseling.
Once everything was taped back together, emergency drawers re-sorted, and at least one teddy bear discharged in stable condition,
my boss approached quietly.
Carefully.
Like someone handling a live grenade with a loose pin.
She put a hand on my shoulder and said, very gently:
“Next time, on your day off… stay home. Please. Don’t answer the phone.”
I nodded.
She nodded.
And without another word, we went back to work.
Because in critical care, that’s just what you do —
whether you’re four years old or thirty-five.
*Disclaimer: This story is entirely fictional. No real toddlers, patients, ICU staff, or crash carts were harmed (permanently) in the making of this article. Any resemblance to real events is purely coincidental… though anyone who’s ever worked in critical care knows it probably wasn’t far off.
If you enjoyed surviving this story with us, follow for more dark ICU humor, battle-worn stories, and caffeinated confessions from behind the sterile curtains.
Want to keep up with our glorious dysfunction? Find us here:
- Facebook — For daily doses of absurdity and low-key trauma bonding.
- Instagram — Behind-the-scenes memes and moral collapse in square format.
- TikTok — Surgical sarcasm with background music and questionable lighting.
Same name everywhere: PropofLOL. Because we don’t just survive medicine — we weaponize it.
